Recently a case of meningitis caused by ear infection in a previously healthy man in the UK made international headlines. In this article I will discuss how an ear infection can cause meningitis.

What is a middle ear infection?
Ear has three parts – external, middle and internal ear. Middle ear is an air filled cavity located in the temporal bone that connects to the nasopharynx(back of the nose) via the eustachian tube on each side. An upper respiratory tract infection can spread to the middle ear via this route. Acute middle ear infection will start with a history of cold, nose block followed by ear pain and fever. It either resolves spontaneously by rupturing through the eardrum or with medical intervention. Rarely ear infection can develop complications such as meningitis.
What is meningitis and can meningitis be caused by ear infection?
Meningitis is the inflammation of the coverings of the brain and spinal cord. There are three layers to meninges from outermost to innermost these are – the dura mater, the arachnoid and the pia mater. Inner two layers i.e. arachnoid and pia mater are called leptomeninges.
Meningitis presents with headache, nausea and vomiting with fever. To understand pathophysiology of meningitis caused by ear infection we need to understand anatomy of ear and its relationship with the brain.
Anatomy of the ear and its relation to the brain
Housed within the temporal bone is the middle and inner ear. Temporal bone is also one of the several bones that form the base of the cranial cavity i.e. the brain rests above the temporal bone.
The following layers separate the ear and the brain:
- Middle ear mucosa
- Tegmen tympani – Bone that forms the roof of middle ear and the floor of cranial cavity
- Dura mater – thick fibrous layer that covers the brain and spinal cord externally
- Arachnoid – vascular layer
- Pia mater – the layer adherent to the brain matter.
Majority of the ear infections heal without any complications with accurate and timely interventions. However, in a small minority the infection can cross the above mentioned layers via direct spread or it may enter the bloodstream causing septicemia and then spread to the brain leading to complications such as meningitis.
Direct spread of infection from ear to brain is more common when there is an infection of the middle ear with a pre-existing erosion of the intervening bony layer i.e. tegmen tympani. This defect could be because of erosion of the bone due to intracranial hypertension, chronic mastoiditis or due to a congenital defect in this layer.
Blood borne spread is more common in acute infections with virulent strains.
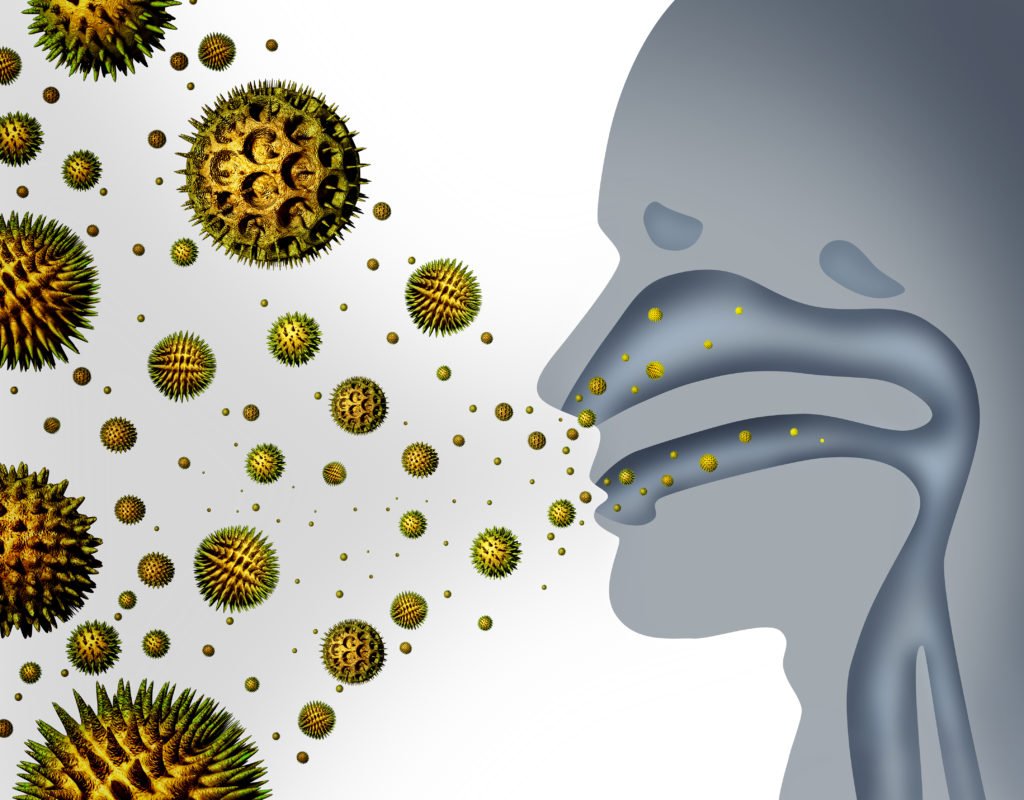
Pathogens that can cause ear infection and meningitis include Neisseria meningitides or Streptococcus pneumoniae both of which are present in the nose, ear and sinuses.
Treatment of meningitis caused by ear infection
A prior history of ear or sinus infections is important for a patient presenting with meningitis. Imaging such as the CT scan or MRI scan of the brain and skull base will show the eroded bony plate and evidence of mastoiditis.
Treatment includes intravenous antibiotics and surgical drainage of the infection, with reconstruction of the tegmen tympani.
Prevention of meningitis
Vaccines against pneumococcal and meningococcal bacteria provide protection against two most common pathogens that cause bacterial meningitis.